3rd December 2019, Care in-between KELP event.
Alexander Graham Bell Conference Centre, Moray College, Elgin.
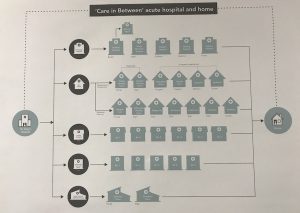
This event was hosted by Glasgow School of Art Design team (GSA) and was attended by a very wide cross-section of people in roles from paramedics and health finance, to those who have experienced using services and care homes. Dr Tara French framed the day by starting to say why GSA was involved in the topic of care ‘in-between’ (this meaning, for example, the space between hospital to home) – GSA initially had started out supporting Moray Health and Social Care around digital design over the last few years and from there this care in-between theme has developed. The GSA team are interested in the design of complex systems, such as health and social care, and innovation within such systems plus their sustainability. Additionally, they are keen to use creativity to transform the system, which we all can agree is needed in these times of great change.
From the start of the day the person (patient) was put at the centre of all design. The workforce was next, how can you support this when such people are under a great deal of pressure. Tara focused us to say this is not so much redesign as reimagining the resources – creating a new vision of what we should be focused toward.
Background on this project: The GSA design team over the last 3-4 month been involved in talking to people as part of their experience of care in-between through interviews, focus groups, and exploratory workshops as well as looking at the data and evidence available from health and social care. “We can’t understand the future until we understand the present” explained Tara.
Four themes were the focus and these were explored by separate groups:
- Transition from Dr Gray’s to home
- Practising person-centred care
- Building resilience through prevention
- Changing perceptions through awareness
Tara made it clear that this was not about finding the solution today to care in-between as this was complex and would take time, but it would take us all further on the journey. She clarified that all of the information shared today will be used in research reporting, shaping the direction of care in-between in Moray, and www.futurehealthandwellbeing.org/moray-integration .
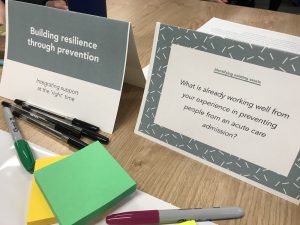 The group I joined was around building resilience and asked the question, “What is already working well from your experience in preventing people from an acute care admission?”
The group I joined was around building resilience and asked the question, “What is already working well from your experience in preventing people from an acute care admission?”
For me I felt that the conversation was very passionate and supportive of a variety of views. We had a good range of people around the table with roles and experiences from areas like Occupational Therapy, mental health, patient involvement, community learning, finance and public health.
There really was far too much to record and reflect on here and this is all recorded on the sheet in the photo. I have to thank our facilitator for doing such an excellent job; our table had some very passionate people (me included) and whilst we were all mindful of one another, the conversation and debates flowed very quickly giving very little chance for breathing never mind recording information.
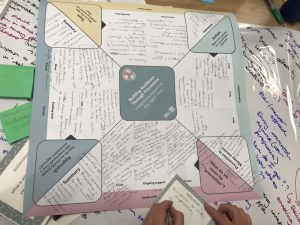
Use of language was an outstanding item, we found that we could not agree or connect on every theme we put forward as individuals, but it felt great to have a shared understanding as a diverse group and a feel for the challenges and what was needed even if we could not articulate it fully yet. One thing we did manage to conclude on was that the group defined prevention as, “building ability to take responsibility without blame and balancing the roles of supporter and supported.” Community connectedness and use of localities was also recognised as important.
Hearing back from the rest of the room as a summary of the morning, what I notice coming up in discussion from other groups was hearing a lot of the same learning that we are experiencing from Moray Wellbeing Hub. For example, there were suggestions of more linking working in hospital to community (rather than it just being a ‘Link Worker’ role) around wellness.
I know that over the last few years I have discussed ideas on having peers in some fashion in Dr Gray’s with a number of people – For example, those with experience of living with colostomy bags to be part of the discharge process for those who now need to use this, meeting people in the hospital and providing peer-support as well as appropriate professional signposting. Or having people at A&E with experience of crisis training to support a compassionate space and signposting at a critical time for people as they wait to see medical professionals, perhaps similar to the wonderful work of the Street Pastors.
Whilst neither idea has come to fruition yet, I know of similar schemes in other places and many supporters and potential collaborators for these projects. I have come to the conclusion, and agree with others who have shared this thought, that an idea is never unique. If you want it realised sharing it widely as well as committing energy to it is the best way forward – fingers crossed sharing it here will stimulate more collaborators and contributors to make it a reality in one way or another (provided it focuses on peer values such as authenticity and mutuality then I am happy!).
There was also talk of recovery planning which made me think about WRAP (Wellness Recovery and Resilience Planning – a course that we deliver when we have resource to do so) and how we can use this more effectively in the future delivery of our Wellness College to give people more access to this kind of tool in a creative and positive way. I decided to bring this back to my delivery team to see if we can do more on this, including supporting care in-between.
Some of the big themes of the session were trust, honest conversations (including ones about what is not possible) and communication as part of this. It made me reflect that the same themes applied internally, within a person or self-talk, were as vital to as those within the system to truly transform change.
“Hospitals are a dangerous place for people to be”, was a great comment that came up a few times. Yes this is often about infection or physical dis-ablement when people get used to being in a bed, but for me it is more for me about the disconnect from CHIME (an acronym for Connectedness, Hope, Identity, Meaning, Empowerment, the evidence base for what works for wellbeing) – your own community and identity, your hopes for the future beyond a diagnosis, feeling empowered to make change in your life (as simple as when you can make a cuppa!) and how to put this experience of a crisis in to context in relation to your wider life.
Part 2: KELP – Keith health centre consultation process.
The second part of the day was looking at the options for a new health centre resource in Keith. There are a number of options already on the table and at this point the team leading this from Health and Social Care Moray needed input from a wider range of views. The bid for the chosen idea will go in the Spring of 2020 to try to attract some funding for the idea and make it a reality. Susan Pellaegrom is the lead in this team and she was keen to stress that there was no funding yet attached to this – idea came first and then, hopefully and not without great effort, the money will follow.
We were given the five options they were currently looking at – new health centre, new health centre with space for multidisciplinary teams, community hub, community elective care and 24hr beds (Susan is keen that if anyone wishes to know more about thes options then to get in touch with her – we can pass on her email).
The group I was in discussed that the purpose of the building was the vital focus, followed closely by the ownership of it by the people of Keith. That it had to be aspirational and ahead of the curve or we would never attract the Scottish Government funding or the pride of local people that is vital to make the long-term success of such a space work.
We spoke about how the project focus needed to decide if it was a wellness or illness space. We agreed that much of the venue will be down to the feel and that we wanted this to be homely. I was able to share some of our feedback from the initial work on the hub from a few years ago and how people wanted a space they walked into that ‘felt like Cheers’ (referring to the 80’s sitcom).
By the end of the session I was fully drained and was glad to be of service to Susan, Tara and the rest of the GSA and KELP project team. Working in true partnership as part of health and social care transformation is a tiring and, as time goes on, more rewarding experience for me. I do feel that the investment of personal resource we as Champions of Moray Wellbeing Hub, peer-activists who use or life experiences as well as professional ones to inform change, put in to health and social care is being met by those who don’t recognise themselves as Champions (yet!); I felt amongst colleagues today, yes there was at least one more visible Champion of the hub in attendance but it was the wider sense of people using all of themselves toward a greater good that was the stronger sensation. Perhaps more people from today will join our social movement, regardless I do think stigma around life challenges (mental health and frailty to name two areas) was challenged as people saw themselves in the system they looked to transform – not as workers but as community members, patients and loved ones.